Payer Solution
Reducing the Burden of Prior Authorization
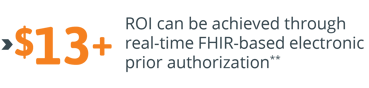
For payers, managing the use of health services requires considerable resources. Prior authorizations (PAs) place a large administrative burden on them as it does for their provider partners. Advancements in medicine, regulations and emerging technology mean payers must navigate increasingly complex medical policy guidelines and standards, making the PA process feel burdensome for their providers and members. Streamlining the PA process can alleviate that burden, giving providers and their members the confidence that they are getting the most appropriate care at the right time. A FHIR-based interoperability approach to PA supports the sharing of specific data needed for the medical necessity review process, leading to faster clinical determinations.
Payers use prior authorization programs selectively to ensure the appropriateness of care delivered and protect member safety.
Key Challenges
For payers, challenges to managing PAs include:
-
Difficulty for providers to confirm the services that require PA
-
Lack of standardized information requirements makes it difficult for providers to understand the required information and results in callbacks for further information
-
Consistent application of medical policies and evidence-based guidelines to each PA
-
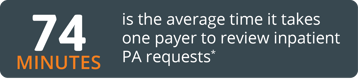
High clinical staffing burn due to long worked hours to meet decision turnaround times
Key Opportunities
-
Reduce staff burden by 70% or more
-
Increase provider satisfaction through real-time determinations and auto approvals
-
Ensure clinical appropriateness through EMR/EHR agnostic clinical data fetch that reduces case review times
-
Improve case turnaround times and compliance
Benefits
-
Increased provider satisfaction through real-time determinations and auto approvals
-
Clear communication of prior authorization requirements and denial rationale
-
Eliminate the need for prior authorization intake and case creation
-
Reduced nurse review time
-
Significant reduction in case turnaround times
-
Improved decision support inter-rater reliability
-
Higher employee satisfaction
Ready to save? Click here to learn more about Smile's Prior Authorization solution.
References
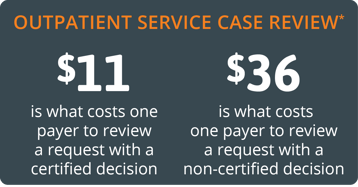
*Case review cost attributed to inpatient specialty services as experienced by one Midwest Commercial Plan.
**Assumes an average case review time of 23 minutes.
