Smile e-Prior Auth: Your Prior Authorization Solution
The Costly Burden of Manual Prior Authorization
In the healthcare industry, manual Prior Authorization (PA) processes have become a significant burden. They lead to delays, frustration, and unnecessary costs for both providers and payers. According to the American Medical Association, 93% of physicians1 report care delays due to Prior Authorization, with an average cost of $13 per manual submission.
The CMS Interoperability 0057F: Why Act Now?
While 2026 may seem distant, the preparations required to meet this mandate are extensive, and time is becoming a scarce resource.
Waiting until 2025, as many organizations might, could be risky. The complexity of ePA (electronic Prior Authorization) implementation may mean that organizations find themselves short of resources and time as the mandate's deadline draws near.
Why Smile e-Prior Auth Solution
✔︎ Streamlined Automation: Smile e-Prior Auth replaces manual Prior Authorization with a streamlined, automated solution, reducing submission times and costs.
✔︎ Real-time Determinations: We provide real-time determinations and auto-approvals, increasing provider satisfaction and ensuring clinical appropriateness.
✔︎ FHIR® and CQL Expertise: As FHIR experts, we align with healthcare standards and mandates, making compliance seamless. Smile Digital Health consistently contributes to the implementation guides (IGs) strongly recommended in mandates, notably the Da Vinci Project.
✔︎ Modular and Comprehensive: We offer a modular solution to fit into your ecosystem with the comprehensiveness of providing you full data support through our Health Data Fabric (HDF).
Learn more about Smile e-Prior Auth solution here
Smile e-Prior Auth Solution Modules for Excellence
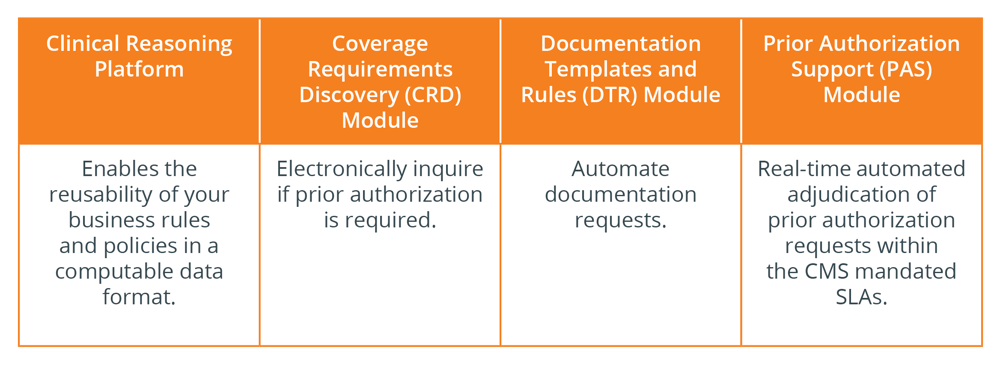
The Total Package for Compliance
Smile offers a comprehensive solution for all CMS mandates, including the Patient Access API, Provider Access API, Payer-to-Payer Solution, and PARDD, and also allows you to scale on the Smile HDF solution that fits right into your ecosystem seamlessly.
Footnotes
